School mental health resources fail students
October 2, 2018
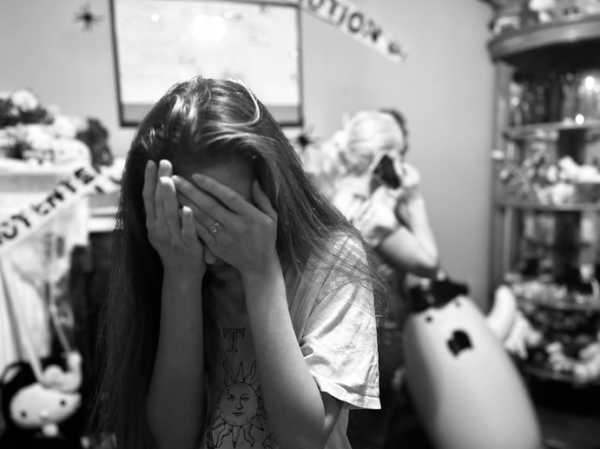
It’s no secret that the American scholastic system faces an epidemic of mentally ill young people, with one in five Americans having mental health problems. Now, America’s high school students are mobilizing in response to school shootings, but a problem more deadly than guns is already in Utah hallways: loopholes in mental health resources.
Suicide has been the leading killer of Utah youth since 2014, and it is growing exponentially. From 2007 to 2017, the CDC found that Utah’s youth suicide rate has nearly tripled, going from 25% more than the national average to nearly 300% of it in 10 years. This takes us from an estimated 180 student deaths per year to nearly 500. The reasons for this increase aren’t clear, but it is certainly enabled by Utah’s counselor-to-student ratio being the third worst in the nation, according to the National School Counselor Association.
The association recommends schools have a 1-250 ratio between school psychologists and students, but the Utah State Board of Education has ruled a 1-350 ratio is “reasonable” for Utah schools, despite nearly doubling the number of students each psychologist attempts to help. “The ratio is reasonable for some areas,” Taylorsville High principal Dr. Garret Muse said, “But not for others.”
However, Utah school districts have failed to meet even these lowered standards with a K-12 average of one counselor for every 725 students, and state high schools are still 40 counselors short of the 1-350 goal. The state legislature compels these schools to change by, “requiring them to submit a plan on how to achieve this ratio.”
Higher student-counselor ratios lead to less individual and group counseling, fewer follow-ups, and a lower standard of care. In fact, the main job of school social workers and psychologists is already to offer “crisis counseling” during available hours for situations of suicide, self-harm, and other immediate circumstances, and to refer students to a third-party counselor covered by family insurance. Non-crisis situations and crises outside of the school social worker’s/psychologist’s hours are handled by academic counselors, the school hope squad, and students are encouraged to speak to teachers.
When asked about the role of schools in offering mental health services, Muse said, “we’re the front line, but we may not be the last line; we stabilize kids and move them on.”
Utah has attempted other mental health measures, such as the SafeUT app, which provides 24/7 crisis counseling via phone for students from the University of Utah’s Neurological ward and alerts school officials of crises, but a student may have to call a different stranger every time they need help. Even free clinics rely on supportive parents driving their kids to their location, or leaving them to walk.
Taylorsville’s AP Psychology teacher, Mrs. Shannon Hanks, said, “some of [treatment] should fall to family, but sometimes the family is the problem, so schools should do whatever we can.”
Crisis options are currently available for students, but resources focused on extremes struggle to follow up and build relationships between students and support. A student with chronic, non-crisis problems may be left behind. As is, our schools respond to mental health problems much like our government: treating the worst symptoms without curing the illness.